A 7-year-old boy with Omnipresent Oedema
This case has been inspired by events in the Torres Straits and details have been changed to ensure patient anonymity.
History
A 7-year-old boy presented to the Primary Healthcare Centre one afternoon after school with his grandmother. She was concerned that his eyes had become quite puffy over the past few days. He had been swimming at the local pool over the weekend and she thought it might be because he had been wearing swimming goggles. He denied any pain around his eyes, diplopia or blurred vision. He also noticed that his school shoes hurt when he put them on.He had no rash, cough, abdominal pain. His bowel and bladder function was normal and hadn’t noticed any recent changes. The patients grandmother commented that he’d had school sores over his legs a few weeks ago. He had no other medical issues, no regular medications or allergies and up to date with immunisations.
Clinical Findings
Observations: BP 140/90, HR 90, RR 20, O2 98% RA, afebrile
(Paediatric BP reference ranges)
Bilateral periorbital & ankle oedema
Heart sounds dual (nil murmurs); Lungs clear (nil creps or wheeze); Abdomen (soft & non-tender)
Remnants of old school sores noted over his lower legs
Urine dipstick ++ blood; ++ protein
What are your differential diagnosis?
How would you approach this patient?
The Case Continued…
We suspected acute post streptococcal glomerulonephritis, not an uncommon occurrence here in the Torres Straits and sent the urine away for microscopy in addition to blood ASO titres, Anti-DNAase B, C3 and renal function. The patient was given IM benzathine penicillin in the clinic and then admitted to hospital for ongoing management.
His initial bloods:
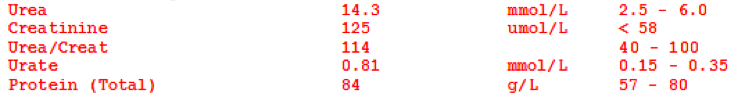
After discussions with our friendly paediatricians in Cairns the patient was commenced on frusemide and an antihypertensive with close fluid monitoring and daily weighs. Our public health nurse was also notified for contact tracing.
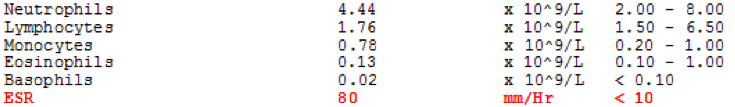
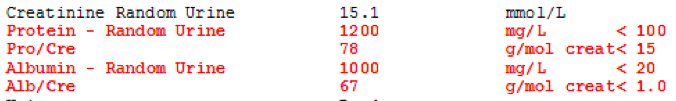
A few days later some more blood results returned, confirming our diagnosis:
![]()
![]()
Pearls from the Torres
Acute post-streptococcal glomerulonephritis (APSGN) is a kidney inflammatory disease which arises as a complication of a group A streptococcal (GAS) skin or throat infection. It is characterised by acute onset oedema, hypertension, haematurea and impaired renal function. In severe cases it can precipitate acute renal failure and hypertensive encephalopathy. APSGN predominantly affects children and is a risk factor for chronic kidney disease later in life. Confirming a case requires both clinical and laboratory evidence.
Clinical evidence (2 or more of the following):
- Hypertension
- Peripheral oedema
- Facial oedema
- Haematurea on urine dipstick
Laboratory evidence:
- Haematuria on microscopy
- Evidence of a recent streptococcal infection (positive Group A Streptococcal culture from skin or throat, or elevated ASO titre or Anti-DNase B)
- Reduced C3 level
All suspected cases of APSGN should be managed under the guidance of your local friendly paediatrician or nephrologist and given IM benzathine penicillin even if skin sores or a sore throat isn’t present at the time of presentation. Prevention of APSGN is achieved by promoting regular washing to reduce bacterial skin load and controlling spread of infected skin sores by treating them with IM benzathine penicillin.

Such interesting information, Ally!
Thank you for sharing❣️