The Torres Approach to Hepatitis B

Chronic hepatitis B (CHB) is widespread in the Torres Strait. Over the last few years there has been a focused effort within the medical team to devise a strategy to ensure safe and appropriate diagnosis and management of CHB. Extensive consultation with the local workforce and relevant specialists guided development of a process to approach CHB in a consistent manner across the region. Importantly, collaboration with local people working in health has ensured the strategy is culturally appropriate and can best improve the health of the community we serve.
Hepatitis B is a virus which can be spread vertically (from mother to baby at birth), horizontally (through household contacts in sharing toothbrushes or razors etc.), through sexual contact and through exposure to infected blood (tattoos, trauma or transfusions). Ninety percent of adults who develop hepatitis B will spontaneously clear the virus, however clearance occurs in only 5% of newborns and 10% of children. A hepatitis B infection which persists for more than six months is defined as chronic hepatitis B. CHB affects approximately 240,000 Australians and about 40% of those are undiagnosed. The effects of CHB infection include development of cirrhosis, liver failure and hepatocellular carcinoma (HCC). Diagnosis and appropriate clinical management of CBH can prevent deaths.
Of the 14,000 people living in the Torres Strait and Northern Peninsula Area 90.7% identify at Aboriginal or Torres Strait Islander (ATSI) persons. It is well documented that ATSI persons are disproportionately affected by CHB. Though this group make up 2.6% of the Australian population, they account for 10% of people living with chronic hepatitis B. The occurrence of HCC in the ATSI population is two to eight times higher than in the general population. Liver related deaths account for 25% of deaths in those with CHB and 70-85% of these deaths are caused by HCC.

As part of a response to improve patient outcomes a clinical guideline was developed. A service evaluation highlighted numerous gaps in the previous approach to CHB in the region, and to address these findings, national guidelines were adapted to be applicable to the remote setting. Extensive consultation with specialists working in gastroenterology, paediatrics, obstetric medicine, sexual health and public health was sought, collaboration with key stakeholders within the local workforce occurred and a standardised approach to management was formulated. Suggested testing and the management of a new diagnosis are outlined below:
Testing:
Testing for hepatitis B is recommended for those in high risk groups. ATSI persons are at an increased risk of CHB. Other high risk groups include those with household or sexual contacts who are positive for hepatitis B, those with chronic liver disease or hepatitis C, migrants from hepatitis B endemic countries and people who inject drugs.
In those at high risk of developing CBH national guidelines suggest testing for hepatitis B surface antigen (HBsAg), hepatitis B core antibody (HBcAb) and hepatitis B surface antibody (HBsAb) at least once in adulthood. HBsAb >10 indicates immunity and if positive no further testing for hepatitis B is required. A positive HBcAb with negative HBsAg and a positive HBsAb infers previous hepatitis B infection which has resolved.
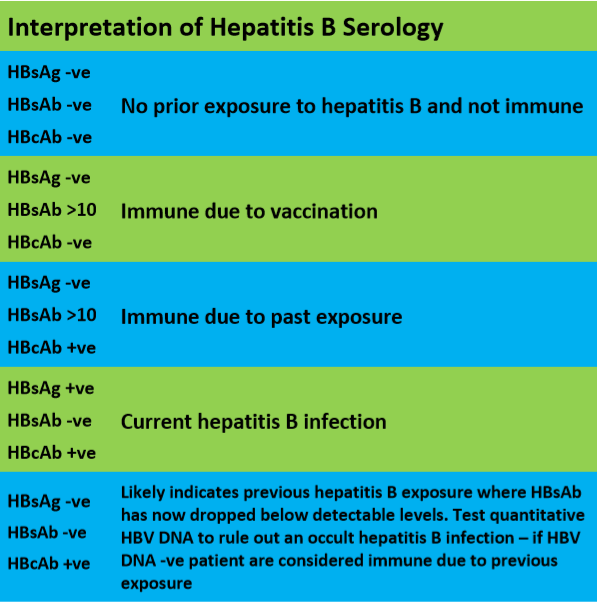
Prior to testing it is important to check previous serology. If at any time in the past a person’s HBsAb >10 no further testing is needed as this proves immunity. Immunity to hepatitis B is to be documented within electronic patient record to avoid unnecessary testing in the future.
Management of a new CHB diagnosis:
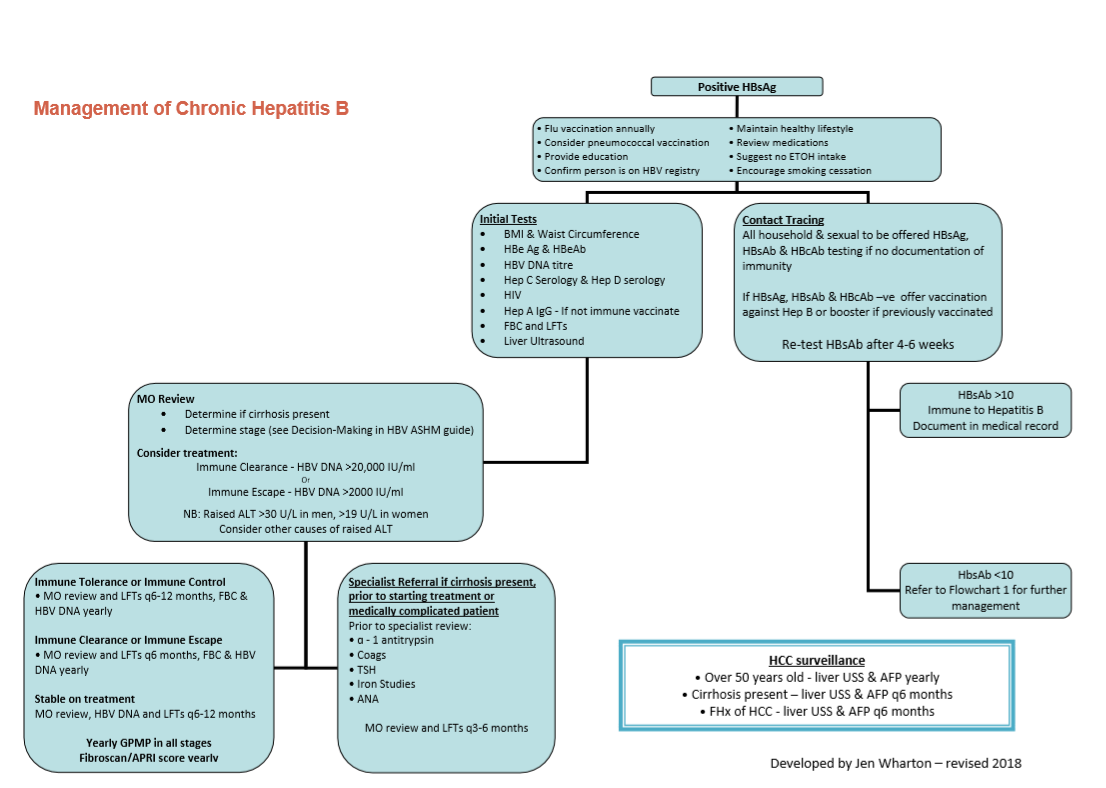
Positive HBsAg indicates a current hepatitis B infection and should HBsAg remain positive for longer than six months this is diagnostic of CHB. All people with CHB should be provided with education regarding their diagnosis, encouraged to maintain a healthy lifestyle, advised to consume no or minimal alcohol and, if relevant, to cease smoking. Annual influenza vaccination is recommended and immunisation against pneumococcal is to be considered. Each new diagnosis should be notified to public health to add to HBV registry. Initial tests and contact tracing are outlined in the flowchart below: Management of Chronic Hepatitis B.
With initial diagnosis all persons should be referred to a medical officer to determine the stage of hepatitis B, perform a medications review, investigate for cirrhosis and consider if antiviral treatment is indicated. Treatment should be considered for those in the immune clearance phase with hepatitis B viral DNA (HBV DNA) levels greater than 20, 000 IU/ml and for those in the immune escape phase at levels above 2000 IU/ml when raised alanine transaminase (ALT) persists for more than 3-6 months. All persons should be offered to participate in developing a GP management plan. A yearly fibroscan or Asparate Transaminase (AST) to Platelet Ratio Index (APRI) score is indicated in all persons for the evaluation of fibrosis. An APRI score <1 is reassuring that fibrosis, and therefore cirrhosis, is unlikely.
Treatment can be commenced by a medical officer with hepatitis B s100 prescribing rights or by a relevant specialist. Specialist opinion for hepatitis B is recommended in cirrhosis, pregnancy or a person who is medically complicated. Tests requested prior to specialist review are outlined in the flowchart below: Management of Chronic Hepatitis B.
At present, five doctors in the Torres are trained hepatitis B s100 prescribers. The ability to initiate and monitor treatment has allowed patients to access appropriate treatment without the need for excess travel away from community to attend specialist appointments. Continuity of care can be provided by local doctors who can include CHB management in the overall care plan collaboratively created with the patient. Close support for hepatitis B s100 prescribers is provided from a group of excellent specialists who are based in Cairns.
The Australian Society of HIV Medicine (ASHM) delivers wonderful training and upskilling to support community prescribers. Upskilling rural generalists in the remote environment has been a great initiative from ASHM and hepatitis B s100 prescriber training has been run on Thursday Island.
The contribution of indigenous health workers in educating the community about hepatitis B is important and has been growing. Indigenous health worker training has been supported by ASHM and culturally appropriate patient information sheets have been developed locally. By equipping indigenous health workers with the skills to educate, contact trace and coordinate care of those with CHB in a culturally-appropriate manner it is hoped patients will benefit by removing a barrier to care.
It is hoped by that by improving clinician knowledge, utilising the skills of the local workforce and visiting specialists, and using a standardised approach to CHB ultimately patients will benefit. At the end of the day, better care and better health outcomes for the community we serve is the reason we are all here.
Resources to Assist Management of Chronic Hepatitis B:
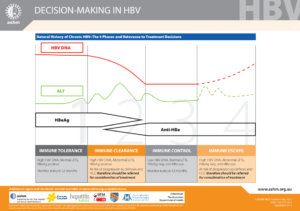
Decision Making in HBV is my most frequently used resource for staging of CHB:
Hepatitis B Australia: B Positive – All you wanted to know about Hepatitis B Treatment, Chronic Hepatitis B, Hepatitis B Diagnosis, and Hepatitis B Management. A guide for Hepatitis B primary care providers.
This awesome patient education website provides information on Hep B, Hep C, HIV and STIs and is presented in Yumplatok (Torres Strait Creole). The content is both written and recorded and available in multiple languages.