Syncope? Think outside the box.
Syncope is a transient and abrupt loss of consciousness with complete return to preexisting neurologic function. It can be classified as neurally mediated (mostly young adults), cardiac, orthostatic, or neurologic.
This case of syncope comes from Faseeh Zaidi, a 5th year medical student studying at the University of Auckland
72-year-old female was brought in by the ambulance after fainting while she was sitting down reading at a cafe. She has had 2-3 other “fainting” events recently all whilst sitting and all with spontaneous recovery. There were no preceding symptoms. There was no head injury. Following the episode, she felt nauseous and light-headed. On admission, she was found to have a prolonged QT and worsening of her hyponatremia.
Past Medical History
1.CVA- old internal capsule infarct
2.Traumatic L5-S1, L1-L2 disc bulge.
3.Neurogenic Bladder with long term indwelling catheter thought secondary to 2.
4. Stage IIIb endometrial adenocarcinoma with completed Surgical management and Chemotherapy
5. Delayed gastric emptying
Admission medications
· Cetirizine 10mg daily
· Omeprazole 20mg daily
· Fluoxetine 20mg daily
· Aspirin 100mg daily
· Nortriptyline 20mg nocte
· Zolpidem 7.5mg nocte
· Metoprolol 23.75mg nocte
· Bendroflumethiazide 2.5mg nocte
· Domperidone 20mg with meals
· Ciprofloxacin 500mg BD long term
Allergies:
· Penicillin – rash
Clinical findings
On general inspection, she felt lightheaded but not disoriented or confused. She had an indwelling suprapubic catheter in place.
Observations: T 35.5, HR 69, BP 154/79, RR 20, SpO2 99% on room air, GCS 15, weight 84kg
Heart sounds dual, no murmurs. Pulse regularly regular. Chest clear, nil added sounds.
Abdomen was soft but mildly tender on palpation over suprapubic area, no signs of peritonism, non-pulsatile and non-expansile abdominal aorta, bowel sounds were present.
Neurological findings were an old right sided facial droop. Coordination and reflexes were intact. Cranial nerves I-XII were intact.
Differential Diagnoses
Syncope due to Cardiac Dysrhythmia especially Long QT
Orthostatic Syncope secondary to Autonomic dysregulation
LOC secondary to Seizure disorder, hyponatremia or CVA
Investigations
Normal WCC, no evidence of sepsis.
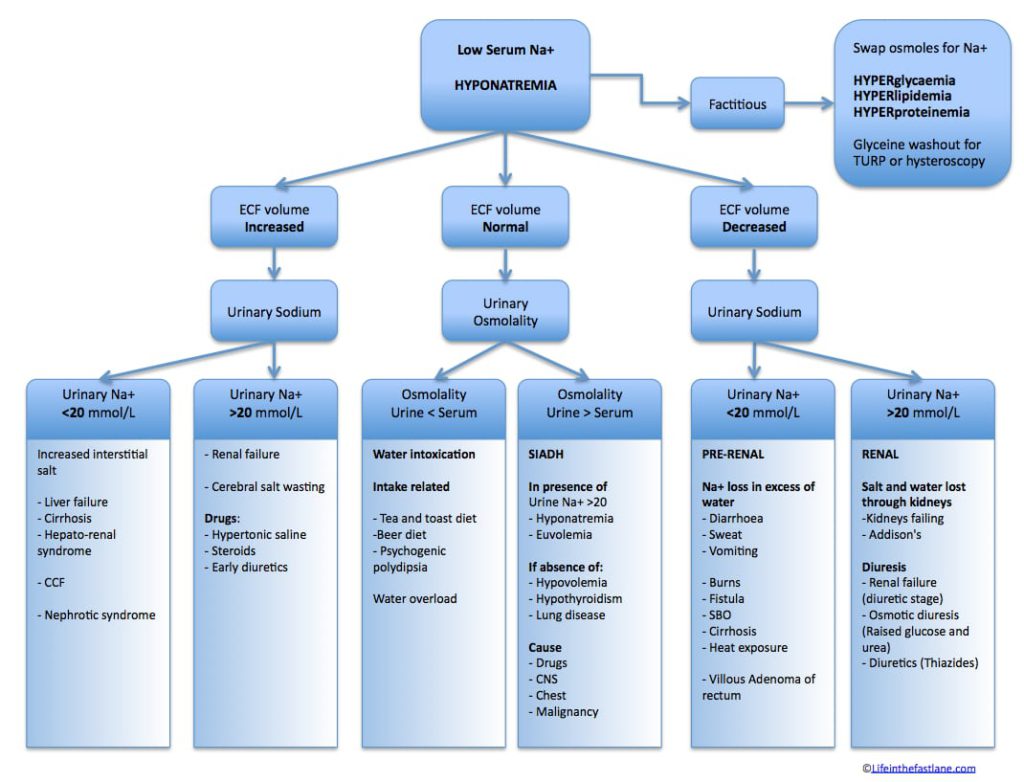
Na 122, K 3.2, Ur 3.2, Cr 44, Glu 6.5 (worsening but not severe hyponatremia, mild hypokalaemia)
CT head showed old left sided internal capsule infarct
The use of thiazide diuretics is a common cause of hyponatraemia. The incidence of hyponatraemia is increasing as a result of guidelines recommending thiazides for the treatment of essential hypertension in many patients. Symptoms include headache, nausea and vomiting, lethargy, and confusion. Seizures, coma, and death may occur in severe cases. Syncope is not typically considered a feature. Thazide diuretics, ACEi and SSRI are common drugs associated with hyponatremia. PPI’s have also been implicated. As has Zolpidem and Ciprofloxacin.
ECG: Normal sinus rhythm at rate 71bpm, normal axis, QTc prolongation at 493ms, no ST abnormalities. An abnormally prolonged QT is associated with an increased risk of ventricular arrhythmias, especially Torsades de Pointes.
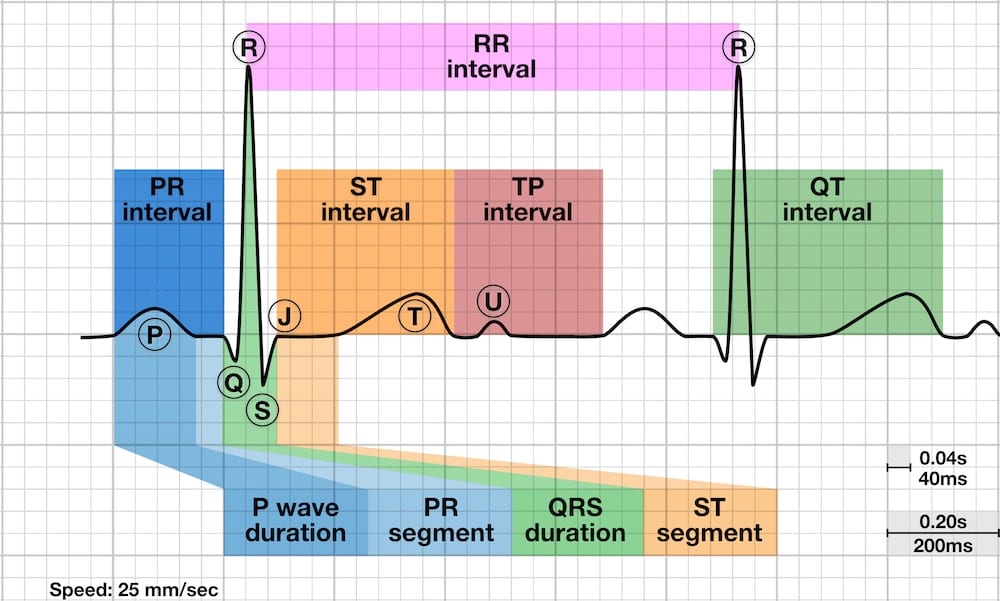
There are multiple formulas used to estimate QTc
Syncope in long QT syndrome can be of neurocardiogenic origin and is not necessarily due to TdP. The reason for neurocardiogenic syncope in this case is unknown, but involvement of the autonomic nervous system outside the heart is possible. In our case the following medications cause prolonged QTc: Fluoxetine, nortriptyline, Zolpidem, Domperidone.
Autonomic dysfunction is the result of a number of disease processes leading to the dis-regulation of the autonomic nervous system:
- Degenerative neurologic diseases, such as Parkinson’s disease.
- An immune-mediated attack as in Guillain-Barre syndrome.
- Metabolic and toxic damage, as in diabetes mellitus or amyloidosis.
- Genetic disorders.
- Abnormal reflex responses in carotid sinus hypersensitivity, vasovagal syncope, and other neuro-meditated syncopes.
- Traumatic or tumoral spinal cord injuries at different levels and presenting with the so-called autonomic dysreflexia
- Pharmacologic effects of several drugs including the toxic effects of chemotherapy.
In this case a number of possibilities are evident with a number of features of autonomic dysregulation, namely neurogenic bladder, delayed gastric emptying and now syncope. There is a past history of spinal cord trauma, a more recent history of chemotherapy and polypharmacy.
Management
During admission, there were no further episodes of syncope.
She was advised to fluid restrict to help with hyponatremia. Medication review in context of both hyponatraemia and QT prolongation. Management of recurrent UTI was discussed with ID Consultant advised cessation of ciprofloxacin, and starting Hiprex (Methanamine) twice daily.
Further management involved ceasing or reducing medications that contributed to her hyponatraemia and prolonged QT; Bendroflumethiazide and Fluoxetine were ceased. Nortriptyline was reduced to 10mg once daily. Metoclopramide was prescribed to replace domperidone.
She has also been referred for out-patient cardiology review with the plan to recommend referral for neurology review should cardiology have nothing further to add.
Thanks to Faseeh Zaidi from Auckland university for providing this case!